The most common causes of lumbar pain are diseases of the spine, especially degenerative-dystrophic diseases (osteochondrosis, spondylosis deformans) and overloading of the back muscles.In addition, various diseases of the abdominal and pelvic organs, including tumors, can cause the same symptoms as a herniated disc that compresses the spinal root.
It is no coincidence that such patients turn not only to neurologists, but also to gynecologists, orthopedists, urologists and, above all, of course, to general practitioners or general practitioners.
Etiology and pathogenesis of lumbar pain
According to modern ideas, the most common causes of pain in the lumbar region are:
- pathological changes in the spine, primarily degenerative-dystrophic;
- pathological changes in the muscles, most commonly myofascial syndrome;
- pathological changes in the abdominal organs;
- Diseases of the nervous system.
Risk factors for lumbar pain include:
- heavy physical activity;
- uncomfortable working posture;
- Injury;
- cooling, drafts;
- alcohol abuse;
- depression and stress;
- Occupational diseases associated with exposure to high temperatures (especially in hot workshops), radiant energy, sudden temperature changes and vibrations.
Vertebral causes of lumbar pain include:
- Root ischemia (discogenic radicular syndrome, discogenic radiculopathy), which results from compression of the root by a herniated disc;
- Reflex muscle syndromes, which can be caused by degenerative changes in the spine.
Various functional disorders of the lumbar spine can play a certain role in the development of back pain if poor posture leads to blockages in the intervertebral joints and their mobility is impaired.Compensatory hypermobility occurs in the joints above and below the block, leading to muscle spasms.
Signs of acute compression of the spinal canal
- Numbness in the perineal area, weakness and numbness in the legs;
- Retention of urination and bowel movements;
- When the spinal cord is compressed, pain relief occurs, followed by numbness in the pelvic girdle and limbs.
Lumbar pain in children and adolescents is usually caused by abnormalities in the development of the spine.Spinal bifida (Spina bifida) occurs in 20% of adults.During the examination, hyperpigmentation, moles, multiple scars and hyperkeratosis of the skin in the lumbar region are revealed.Sometimes urinary incontinence, trophic disorders and weakness in the legs are noted.
Pain in the lumbar spine can be caused by lumbarization - the junction of the S1 vertebra in relation to the lumbar spine - and sacralization - the attachment of the L5 vertebra to the sacrum.These anomalies arise due to individual features of the development of the transverse processes of the vertebrae.
Nosological forms
Almost all patients complain of pain in the lower back.The disease manifests itself primarily through inflammation of the difficult-to-move joints (intervertebral, costal and lumbar vertebral joints) as well as the ligaments of the spine.Gradually, ossification develops in them, the spine loses elasticity and functional mobility, becomes like a bamboo stick, brittle and can be easily injured.At the stage of pronounced clinical manifestations of the disease, the mobility of the chest during breathing and, as a result, the vital capacity of the lungs decreases significantly, which contributes to the development of a number of pulmonary diseases.
Spinal tumors
A distinction is made between benign and malignant tumors, which primarily originate in the spine and metastasize.Benign tumors of the spine (osteochondroma, chondroma, hemangioma) are sometimes clinically asymptomatic.With hemangioma, even minor external influences can cause a spinal fracture (pathological fracture).
Malignant tumors, usually metastatic, arise in the prostate, uterus, breast, lungs, adrenal glands and other organs.Pain in this case occurs much more often than with benign tumors - usually persistent, painful, intensifying with the slightest movement and depriving the patient of rest and sleep.Characterized by a progressive deterioration of the condition, an increase in general fatigue and pronounced changes in the blood.X-rays, computer tomography and magnetic resonance imaging are of great importance for diagnostics.
osteoporosis
The main cause of the disease is a deterioration in the functioning of the endocrine glands due to an independent disease or against the background of general aging of the body.Osteoporosis can develop in patients who take hormones, aminazine, anti-tuberculosis drugs and tetracycline for a long time.Radicular diseases, which are associated with back pain, arise from deformation of the intervertebral foramina, and spinal diseases (myelopathy) arise from compression of the radiculomedullary artery or vertebral fracture, even after minor injuries.
Myofascial syndrome
Myofascial syndrome is the main cause of back pain.It can occur due to overexertion (during heavy physical activity), overstretching and muscle bruises, unphysiological posture during work, reaction to emotional stress, shortening of a leg and even flat feet.
Myofascial syndrome is characterized by the presence of so-called “trigger” zones (trigger points), the pressure of which causes pain that often radiates to neighboring areas.In addition to myofascial pain syndrome, pain can also be caused by inflammatory muscle diseases – myositis.
Lumbar pain often occurs due to diseases of internal organs: stomach and duodenal ulcers, pancreatitis, cholecystitis, urolithiasis, etc. They can be pronounced and mimic the picture of lumbago or discogenic lumbosacral radiculitis.However, there are also clear differences that allow referred pain to be distinguished from pain resulting from diseases of the peripheral nervous system that are due to the symptoms of the underlying disease.
Clinical symptoms of lumbar pain
Lumbar pain most commonly occurs between the ages of 25 and 44.There is acute pain, which usually lasts 2-3 weeks and sometimes up to 2 months, and chronic pain – over 2 months.
Radicular compression syndromes (discogenic radiculopathy) are characterized by a sudden onset, often following heavy lifting, sudden movements, or hypothermia.Symptoms depend on the location of the lesion.The appearance of the syndrome is due to the compression of the root by a herniated disc, which occurs as a result of degenerative processes promoted by static and dynamic loads, hormonal disorders and injuries (including microtraumatization of the spine).Most often, the pathological process affects areas of the spinal roots from the dura mater to the intervertebral foramen.In addition to a herniated disc, bone growth, scarring changes in the epidural tissue, and a hypertrophied ligamentum flavum can also be involved in root trauma.
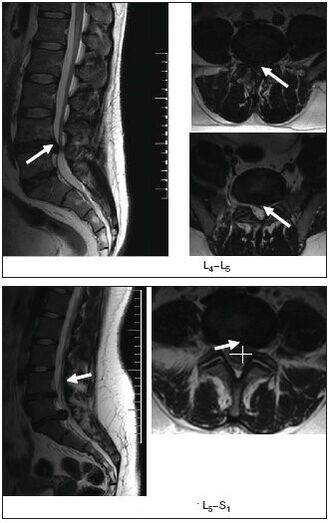
The upper lumbar roots (L1, L2, L3) are rarely affected: they account for no more than 3% of all lumbar radicular syndromes.The L4 root is affected twice as often (6%), resulting in a characteristic clinical picture: mild pain along the inner, lower and anterior surface of the thigh, the medial surface of the leg, paresthesia (numbness, burning, crawling) in this area;slight weakness of the quadriceps muscle.The knee reflexes are preserved and sometimes even increased.The L5 root is most commonly affected (46%).The pain is localized in the lumbar and buttocks, along the outer surface of the thigh, the anterior outer surface of the lower leg to the foot and fingers III-V.It is often accompanied by a decrease in the sensitivity of the skin on the anterior surface of the leg and the strength of the extensor muscles of the third to fifth fingers.The patient finds it difficult to stand on his heels.With long-standing radiculopathy, hypotrophy of the tibialis anterior muscle develops.The S1 root is also often affected (45%).In this case, pain in the lower back radiates along the outer back of the thigh, the outer surface of the lower leg and the foot.Examination often reveals hypalgesia of the posterior external surface of the leg, reduced strength of the triceps muscle and toe flexors.It is difficult for such patients to stand on tiptoes.There is a decrease or loss of the Achilles tendon reflex.
Vertebrogenic lumbar reflex syndrome
It can be acute or chronic.Acute lumbar pain (LBP) (lumbago, “lumbago”) occurs within minutes or hours, often suddenly due to uncomfortable movements.The sharp, stabbing (like an electric shock) pain is localized throughout the lower back and sometimes radiates to the pelvic region and buttocks.It increases greatly when coughing and sneezing and decreases when lying down, especially if the patient finds a comfortable position.The ability to move the lumbar spine is limited and the lumbar muscles are tense, leading to Lasegue symptoms that often occur on both sides.The patient lies on his back with his legs stretched out.At the same time, the doctor bends the affected leg at the knee and hip joints.This does not cause any pain because this leg position relaxes the affected nerve.Then the doctor begins to leave the leg bent at the hip-thigh joint, straightening it at the knee, which tenses the sciatic nerve, which causes severe pain.Acute lumbodynia usually lasts 5-6 days, sometimes less.The first attack ends faster than the following ones.Repeated attacks of lumbago tend to develop into chronic LBP.
Atypical lower back pain
There are a number of clinical symptoms that are atypical of back pain caused by degenerative changes in the spine or myofascial syndrome.These characters include:
- the occurrence of pain in childhood and adolescence;
- Back injury just before lower back pain begins;
- Back pain accompanied by fever or symptoms of intoxication;
- spine;
- rectum, vagina, both legs, girdle pain;
- Association of lower back pain with eating, bowel movements, sexual intercourse, urination;
- non-ecological pathology (amenorrhea, dysmenorrhea, vaginal discharge), which occurred against the background of pain in the lower back;
- increased pain in the lower back in a horizontal position and decreased pain in a vertical position (Razdolsky symptom, characteristic of a tumor process in the spine);
- steadily increasing pain over one to two weeks;
- Limbs and the appearance of pathological reflexes.
Investigation methods
- External examination and palpation of the lumbar spine, identification of scoliosis, muscle tension, pain and trigger points;
- Determination of the range of motion of the lumbar spine, areas of muscle loss;
- Examination of neurological status;Determination of tension symptoms (Lassegue, Wasserman, Neri).[Examination of Wasserman's symptom: Bending the leg at the knee joint in a patient in the prone position causes pain in the thigh.Examination of Neri's symptom: A sharp bend of the head to the chest of a patient lying on his back with his legs straight causes acute pain in the lower back and along the sciatic nerve.];
- Examination of the state of sensitivity, reflex sphere, muscle tone, vegetative disorders (swelling, color changes, temperature and humidity of the skin);
- X-ray, computer or magnetic resonance imaging of the spine.
MRI is particularly informative
- Ultrasound examination of the pelvic organs;
- gynecological examination;
- If necessary, additional examinations are carried out: cerebrospinal fluid, blood and urine, sigmoidoscopy, colonoscopy, gastroscopy, etc.
Treatment
Acute low back pain or exacerbation of vertebral or myofascial syndromes
Undifferentiated treatment.Gentle engine mode.If the pain is severe in the first few days, rest in bed and then walk on crutches to relieve the pressure on the spine.The bed should be hard and there should be a wooden board under the mattress.For warmth, a wool scarf, an electric heating pad, and bags of heated sand or salt are recommended.Ointments have a beneficial effect: Finalgon, Tiger, Capsin, Diclofenac, etc., as well as mustard plasters and pepper plasters.UV irradiation in erythematous doses, leeching (taking into account possible contraindications) and rinsing the painful area with ethyl chloride are recommended.
Electrical procedures have an analgesic effect: transcutaneous electroanalgesia, sinusoidally modulated currents, diadynamic currents, electrophoresis with novocaine, etc. The use of reflexology (acupuncture, laser therapy, cauterization) is effective;Novocaine blockades, pressure massage of trigger points.
Drug therapy includes analgesics, NSAIDs;sedatives and/or antidepressants;Medicines that reduce muscle tension (muscle relaxants).In case of arterial hypotension, tizanidine should be prescribed with great caution due to its antihypertensive effect.If swelling of the spinal roots is suspected, diuretics are prescribed.
The main analgesics are NSAIDs, which are often used uncontrollably by patients when pain increases or recurs.It should be noted that long-term use of NSAIDs and analgesics increases the risk of complications from this form of therapy.There is currently a wide range of NSAIDs.For patients with spinal pain, diclofenac 100-150 mg/day are the preferred “non-selective” drugs due to availability, effectiveness and lower likelihood of side effects (gastrointestinal bleeding, dyspepsia).oral, intramuscular, rectal, local, ibuprofen and ketoprofen oral 200 mg and topical and among the “selective” – meloxicam oral 7.5-15 mg/day, nimesulide oral 200 mg/day.
Side effects may occur during treatment with NSAIDs: nausea, vomiting, loss of appetite, pain in the upper abdomen.Possible ulcerogenic effect.In some cases, ulcers and bleeding in the gastrointestinal tract may occur.In addition, headaches, dizziness, drowsiness and allergic reactions (skin rash, etc.) are noted.Treatment is contraindicated in ulcerative processes in the gastrointestinal tract, pregnancy and breastfeeding.To prevent and relieve dyspeptic symptoms, it is recommended to take NSAIDs and drink milk during or after meals.In addition, as in the long-term treatment of many chronic diseases, the use of NSAIDs when pain increases together with other medications that the patient is taking to treat concomitant diseases leads to reduced adherence to therapy and, as a result, to insufficient effectiveness of the therapy.
Therefore, modern methods of conservative treatment include the mandatory use of drugs that have chondroprotective, chondrostimulating effects and have a better therapeutic effect than NSAIDs.The drug Teraflex-Advance fully meets these requirements and is an alternative to NSAIDs for mild to moderate pain.One capsule of the drug Teraflex-Advance contains 250 mg of glucosamine sulfate, 200 mg of chondroitin sulfate and 100 mg of ibuprofen.Chondroitin sulfate and glucosamine are involved in the biosynthesis of connective tissue and help prevent cartilage destruction processes and stimulate tissue regeneration.Ibuprofen has pain-relieving, anti-inflammatory and fever-reducing effects.The mechanism of action is based on the selective blocking of cyclooxygenase (COX types 1 and 2), the main enzyme in the metabolism of arachidonic acid, which leads to a reduction in prostaglandin synthesis.The presence of NSAIDs in the composition of the drug Theraflex-Advance helps to increase the range of motion of the joints and reduce morning stiffness of the joints and spine.It should be noted that according to R.J.According to Tallarida et al.The presence of glucosamine and ibuprofen in Theraflex-Advance ensures a synergism in terms of the analgesic effect of the latter.In addition, the analgesic effect of the glucosamine/ibuprofen combination is achieved by a 2.4-fold lower ibuprofen dose.
After pain relief, it makes sense to switch to taking the drug Teraflex, which contains the active ingredients chondroitin and glucosamine.Teraflex is taken 1 capsule three times a day.during the first three weeks and 1 capsule twice daily.in the next three weeks.
The vast majority of patients taking Theraflex experience positive dynamics in the form of pain relief and a reduction in neurological symptoms.The drug was well tolerated by patients, no allergic manifestations were detected.The use of Teraflex for degenerative diseases of the spine is particularly useful in young patients, both in combination with NSAIDs and as monotherapy.In combination with NSAIDs, the analgesic effect occurs twice as quickly and the need for therapeutic doses of NSAIDs progressively decreases.
In clinical practice, for lesions of the peripheral nervous system, including those associated with spinal osteochondrosis, B vitamins are often used, which have a neurotropic effect.Traditionally, the method of alternating administration of vitamins B1, B6 and B12 at 1-2 ml each is used.intramuscularly alternating daily.The treatment period is 2-4 weeks.The disadvantages of this method include the use of small doses of medication, which reduces the effectiveness of treatment and the need for frequent injections.
Traction therapy is used for discogenic radiculopathy: traction (including underwater) in a neurological clinic.With myofascial syndrome, after local treatment (novocaine blockade, rinsing with ethyl chloride, anesthetic ointments), a hot compress is applied to the muscles for several minutes.
Chronic lumbar pain of vertebrogenic or myogenic origin
In the event of a herniated disc, the following is recommended:
- wearing a rigid corset such as a “weightlifting belt”;
- Avoid sudden movements and bending and limit physical activity.
- Physiotherapy to create a muscle corset and restore muscle mobility;
- Massage;
- novocaine blockades;
- reflexology;
- Physiotherapy: ultrasound, laser therapy, heat therapy;
- intramuscular vitamin therapy (B1, B6, B12), multivitamins with mineral supplements;
- For paroxysmal pain, carbamazepine is prescribed.
Non-drug treatments
Despite the availability of effective means of conservative treatment and the existence of dozens of techniques, some patients require surgical treatment.
The indications for surgical treatment are divided into relative and absolute indications.The absolute indication for surgical treatment is the development of caudal syndrome, the presence of a sequestered disc herniation and severe radicular pain syndrome that does not subside despite treatment.The development of radiculomyeloischemia also requires emergency surgical intervention, although in such cases the indications for surgery diminish after the first 12-24 hours, on the one hand due to the formation of irreversible changes in the roots and on the other hand because the process resolves in most cases within approx. 6 months as part of treatment and rehabilitation measures.The same regression periods are observed in delayed operations.
Relative indications include failure of conservative treatment and recurrent sciatica.The duration of conservative therapy should not exceed 3 months.and lasts for at least 6 weeks.It is assumed that in the case of acute radicular syndrome and failure of conservative therapy within the first 3 months, a surgical procedure is justified.after the onset of pain in order to prevent chronic pathological changes in the root.A relative indication is cases of extremely severe pain syndrome, in which the pain component is replaced by an increase in neurological deficit.
Among the physiotherapeutic procedures, electrophoresis with the proteolytic enzyme caripazim is currently often used.
It is known that therapeutic physical training and massage are an integral part of the complex treatment of patients with spinal lesions.Remedial gymnastics aims to generally strengthen the body, increase performance, improve movement coordination and increase fitness.In this case, special exercises are aimed at restoring certain motor functions.




















